
Scientists embedded sensors in a face mask to diagnose kidney disease. (Yuganov Konstantin/Shutterstock)
In a nutshell
- A sensor-equipped face mask detected chronic kidney disease (CKD) with over 93% accuracy by analyzing compounds in a person’s breath, offering a potential alternative to invasive blood tests.
- The mask identifies a “breath fingerprint” of CKD, including elevated levels of ammonia, acetone, and other compounds that build up when the kidneys aren’t functioning properly.
- Researchers say this wearable technology could one day monitor disease progression non-invasively, making it easier to track kidney health in real time, especially in low-resource settings.
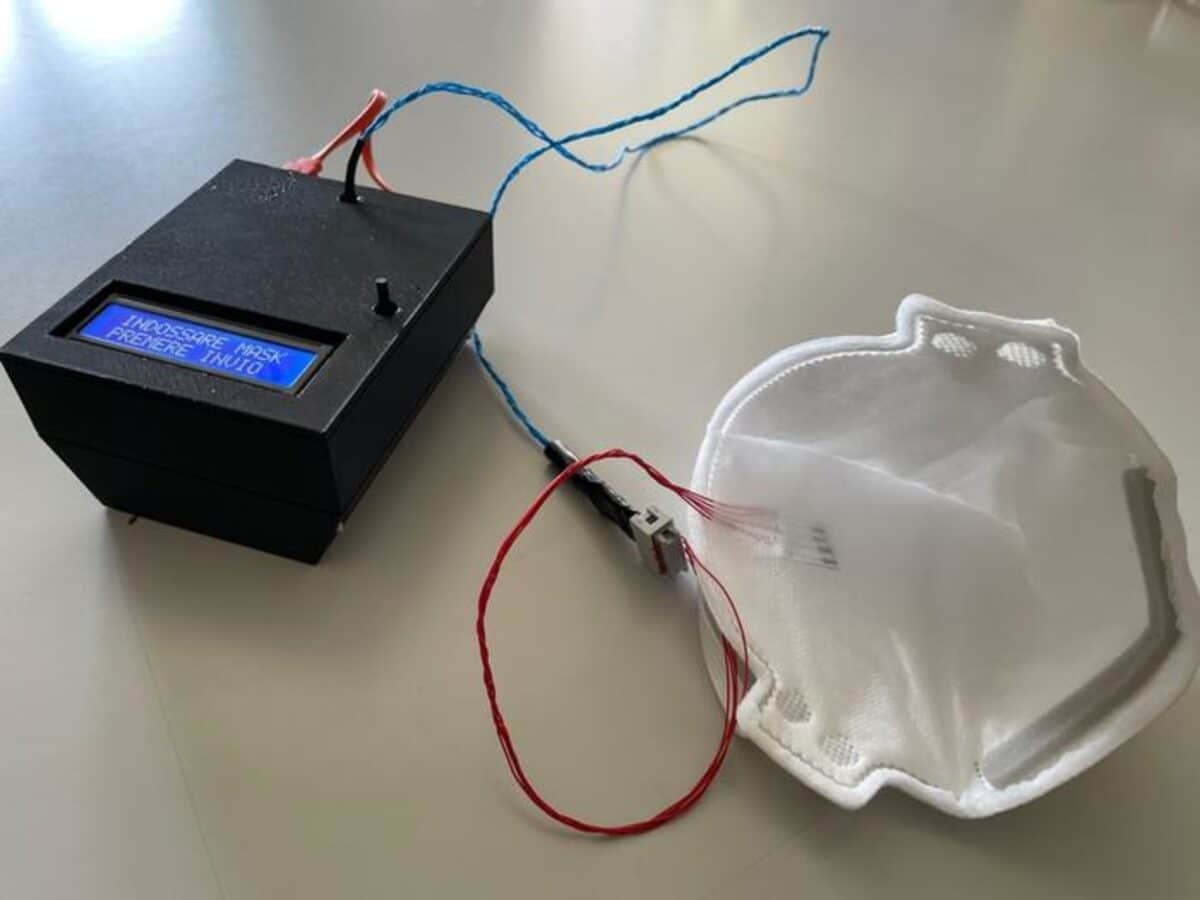
ROME, Italy — Forget invasive blood tests and expensive doctor visits; your breath might hold the key to monitoring kidney disease. Scientists from Italy have cleverly repurposed the humble face mask, embedding it with four sensitive gas detectors that can identify chronic kidney disease by analyzing the chemical compounds you exhale. This wearable technology correctly spotted kidney disease patients with over 93% accuracy, pointing toward a future where disease monitoring becomes as natural as breathing.
In a recent study published in ACS Sensors, researchers embedded tiny gas sensors into ordinary FFP2 face masks that can detect subtle changes in breath composition linked to kidney function. The innovative design shows remarkable potential for transforming how we approach kidney disease, a condition affecting approximately 10% of the global population.
The growing worldwide impact of chronic kidney disease makes it essential to create basic and cost-effective diagnostic methods. Their approach takes advantage of the connection between breath composition and kidney disease, using sensors that detect ammonia and other substances that increase when kidneys aren’t functioning properly.
For the millions of people living with CKD worldwide, this technology could represent a significant advancement in how the disease is detected and monitored. Current diagnostic methods typically require blood tests and urine analysis, which can be invasive, time-consuming, and costly, particularly in resource-limited settings.
How Breath Sensors Detect Kidney Disease
Adapted from ACS Sensors 2025, DOI: 10.1021/acssensors.4c03227)
The research team created a system of four gas sensors made from porphyrins (molecular compounds similar to those found in hemoglobin) combined with a conductive polymer called PEDOT/PSS. These materials were printed onto a flexible substrate and tucked into the inner layer of standard FFP2 masks, where they could continuously monitor the wearer’s exhaled breath without adding bulk or discomfort.
When our kidneys begin to fail, various compounds start to accumulate in the bloodstream instead of being filtered out through urine. Some of these compounds, particularly ammonia, eventually find their way into our breath. Previous research has shown that people with CKD have ammonia breath concentrations of approximately 34 parts per million compared to just 2.9 parts per million in healthy individuals.
However, ammonia isn’t the only marker. Other compounds like trimethylamine, acetone, and dimethyl sulfide also increase in the breath of kidney disease patients. This complex mixture of compounds creates a unique “breath fingerprint” that the sensor array was designed to detect.
Each of the four sensors in the array responds differently to various chemical compounds. Two contained free-base porphyrins that showed the highest sensitivity to ammonia, while two others contained manganese-modified porphyrins that were more responsive to alcohols and other compounds. This diversity allowed the array to capture a broad picture of breath composition rather than relying on a single biomarker.
To use the device, participants simply wore the mask and followed a specific breathing protocol, first breathing normally for about a minute, then slightly accelerating their breathing rate for another minute. This approach helped standardize the measurements and overcome one of the key challenges in breath analysis: the lack of a reference gas to compare against.
93% Detection Accuracy
The research team recruited 101 participants, including 53 CKD patients at various stages of the disease and 48 healthy controls. The groups were matched for age and gender to minimize demographic variables that might affect the results.
Before testing, participants were asked to refrain from eating, drinking (except water), and smoking for two hours. After rinsing their mouths, they donned the sensor-equipped masks and performed the specified breathing patterns while the device recorded data.
When analyzing the results, the team found that their system could distinguish between CKD patients and healthy controls with remarkable accuracy. Using a statistical approach called linear discriminant analysis (LDA), the system achieved 93.3% true positives (correctly identifying CKD patients) and 86.7% true negatives (correctly identifying healthy controls).

The sensor array might also be able to classify patients according to the severity of their kidney disease, potentially allowing doctors to monitor disease progression without repeated blood tests. This could be particularly valuable for tracking patients over time and adjusting treatments accordingly.
This technology represents a significant step forward in non-invasive medical testing. Unlike traditional diagnostic methods for kidney disease, which require blood draws and laboratory analysis, the mask-based sensor could potentially provide continuous, real-time monitoring with minimal disruption to daily life.
The researchers see this as just the beginning. Their findings suggest that with proper expansion of the sensor array, these specially equipped facemasks might potentially be used to diagnose a wider range of diseases and conditions. Similar technology could eventually detect other conditions with breath biomarkers, such as diabetes, liver disease, or certain types of cancer.
The approach also takes advantage of a now-familiar accessory. After the widespread adoption of face masks during the COVID-19 pandemic, integrating medical sensors into these devices feels like a natural progression. The masks provide an ideal platform for breath analysis, as they naturally capture exhaled breath in a confined space close to the source.
For patients with chronic conditions requiring ongoing monitoring, this type of technology could significantly reduce healthcare costs while improving quality of life. While most of us hoped to move beyond masking after the pandemic, this research suggests that masks might actually become an invaluable part of healthcare’s future, not just blocking pathogens from getting in, but detecting disease markers coming out.
Paper Summary
Methodology
Researchers developed an array of four resistive gas sensors using blends of porphyrins and PEDOT/PSS conducting polymer, printing them on flexible substrates and embedding them in standard FFP2 face masks. The sensors were designed to detect ammonia and other volatile compounds associated with kidney disease. The clinical study enrolled 101 participants (53 CKD patients and 48 healthy controls) who were asked to wear the sensorized masks and perform two breathing cycles at different rates. Sensor signals were processed using continuous wavelet transform to extract features, which were then analyzed using hierarchical cluster analysis, principal component analysis, and linear discriminant analysis.
Results
The sensor array successfully distinguished between CKD patients and healthy controls with high accuracy. The linear discriminant analysis achieved 93.3% true positives and 86.7% true negatives. Additionally, the system showed potential for stratifying patients according to disease severity, with statistical differences observed between different CKD stages. The sensors demonstrated high sensitivity to ammonia and other relevant volatile compounds, with each sensor exhibiting a distinct pattern of sensitivity that contributed to the overall discriminatory power of the array.
Limitations
The study acknowledged that the sample size for each CKD stage was relatively small, which limited the reliability of classification algorithms for disease staging. The technology also requires specific breathing protocols to standardize measurements, which might be challenging for some patients to follow precisely. While the current prototype showed promising results, the researchers noted that expansion of the sensor array would be beneficial for broader disease detection capabilities.
Funding and Disclosures
The research was supported by the European Union—NextGenerationEU (project ECS 0000024 Rome Technopole). The experimental protocol complied with the 1975 guidelines of the Declaration of Helsinki and was approved by the Independent Ethics Committee of the Policlinico Tor Vergata. All participants provided written informed consent before participation in the study.
Publication Information
The paper titled “Disposable Sensor Array Embedded in Facemasks for the Identification of Chronic Kidney Disease” was published in ACS Sensors on April 17, 2025. The research was conducted by a team from the University of Rome Tor Vergata, led by corresponding author Corrado Di Natale, with contributions from multiple departments including Electronic Engineering, Chemical Science and Technologies, Systems Medicine, and Experimental Medicine.







